 This is my first blog post ever! I consider this another gift of the pandemic.
This is my first blog post ever! I consider this another gift of the pandemic.
When I reflect on the last year, I have a hefty share of good memories. Of coming home after work, sans planned social activities, and immersing myself in a landscaping project in my backyard. I dug up old bricks – they must have been walkways or something at one point – to use as borders for new plots I’d carved for mulching and planting blooming things. In my “normal” life, this would have felt like a chore, because I would have been trying to squeeze it in on weekends or random week nights between other things I was running around doing. Instead, I sat in the grass and patiently outlined the new beds and placed each brick one by one, just how I wanted them. It was a time of peace and reflection, drenched as I was in the smells and the sounds and the feeling of spring.
I found myself calling and FaceTiming with family and old friends a lot more than I had in the past. They mostly live in Tennessee, so I wouldn’t have been regularly seeing them in person even in pre-pandemic life, but somehow now the interactions felt deeper and I was more invested.
I very much enjoyed walking and running outdoors over the spring and summer. Suddenly, there was hardly any traffic and I didn’t encounter a bunch of college students crossing my path, so although I still had a mask that I’d pull up when I encountered someone, I felt pretty relaxed when I ventured out into this city I love.
When I was asked to write to IPA members through this forum as we reflect on the last year, I was enthused. I don’t normally think back on distinct periods of time in my life regarding challenges and changes; I’m more the type to suddenly realize that things have shifted over time. In this case, the pandemic has conveniently provided a clear-cut timeframe in which to examine the good and the bad and the in-between of life.
I am speaking to a wide array of you, my IPA colleagues, so initially I thought about writing from the perspective of “us” and how “we” have been affected. I do feel affiliated with all of you, but I realized I can only speak with my singular voice, and hope that my reflections resonate with you in some way. I will point out a couple of things about me that make me and my experience possibly different from yours:
I am single and live alone (with the exception of pets) so home life didn’t change for me.
I am a psychologist in a niche part of healthcare that didn’t shut down with the shutdown.
I know a lot of you have families with spouses and children who have needed a lot of care at home, and negotiation of time and space with everyone together, and this has likely put an extra burden on you as you’ve navigated these situations. I feel for you. I know also that many of you must have been very concerned about your jobs when this started, wondering if you were going to be able to pay bills or whether your practices would survive. One year later, I hope those issues are getting more manageable, especially with the gift of telehealth.
Though I found much to treasure in my home life once the pandemic started, I struggled in my work. As I mentioned, my job didn’t allow for pauses when the coronavirus hit, so I reluctantly put on a mask and face shield and sat in a clinic room too small to accommodate six feet of social distancing. I see immunocompromised patients who I assumed were shedding COVID and many other germy particles all over the floor, furniture, and in my general direction. I doused my dry and cracking hands in alcohol constantly and kept disinfecting wipes in my car. I tried to wipe everything down once home at the end of the day, including things I don’t normally think about touching, like the handle on the turn signal and the garage door opener. It awakened me to my own daily habits, behaviors that usually exist well below my conscious awareness. I was actually intrigued by this, my new awareness of myself.
I observed something in my perception of and attitude towards my role as a psychologist in those early days, something that truly disturbed me: before the pandemic I welcomed the opportunity to meet a new patient/client so that I might enter into their fear and uncertainty and help them feel less alone, to provide validation, help them see opportunities instead of endings, and hopefully start the work of finding meaning in the struggle, and identify the small sparks of hope and intention to propel them in their movement back to health. Now I saw them as a threat. To me. They could sicken me. They could kill me.
I dreaded that entry to the room, my face masked and head bound in a wrap to protect my skin and ears from the discomfort of the heavy face shield with its thick plate of plastic covering my face and the top of my head. (The ray of sunshine in this: the generous people in our community to who made and donated the shields and homemade masks.) I was wearing what felt like war armor and the situation felt adversarial. I resented that I had to spend time in that closed space with these people, neither of us able to hear each other because my words bounced off the plastic back in my face when I spoke, and I couldn’t hear them because of their masks and my ears being partially covered. Their masks also denied me the opportunity to use their expressions for context and understanding of what they shared, so we essentially yelled at each other. (Compassion doesn’t feel so compassionate at certain volumes!) I might note that they didn’t want to be with me or in that room either, fearing their exposure to the germy stuff floating around the hospital. We finished up our sessions as quickly as possible. It didn’t feel therapeutic. It felt the opposite of therapeutic, in fact.
I’d go home with headaches almost every day. I have observed that our neck muscles are perfectly designed to hold the weight of our skulls and the contents within, accommodating various degrees of hair/hairlessness, and that’s it. Any added weight is simply too much weight. I went home with headaches and muscle tension in my shoulders daily. Did. Not. Improve. My. Attitude. But within this came another ray of light: the creative souls in our world designed awesome lightweight shields to help those required to wear them. This pandemic gave me, a highly independent do-it-yourselfer, a chance to rely on the ingenuity of others. It was an important and humbling reminder that we need each other.
The masks keep us safe but only impede communication, for sure. In-person sessions have changed. (One of many gifts of telehealth: seeing a person’s whole face!) Some people are simply not terribly expressive through their eyes, eyebrows, and forehead. I’ve spoken to patients who appeared dysphoric and flat to me, only to be surprised when he chuckles over something or she hoots with laughter while telling me about her day. I miss the small grins, the big, toothy smiles, the quiver of the lips when something sensitive comes up. Those big and little facial movements that provide such richness in our non-verbal communication are gone. I still can’t help myself from smiling at people when I pass them in the halls or enter a clinic room or when I make an infrequent trip to the grocery store. I envy those people who have mastered the art of making eye contact and giving the friendly nod. I’m not a nodder. I crinkle in response. I love the nodders. They make me happy.
It’s so very important to speak more now. This is not a bad thing: to check in with people in the present, to ask more questions, to describe feelings and reactions. Thank you, pandemic.
Telehealth is an interesting beast. Technology of this sort is not intuitive to me. I’ve had to be walked through every aspect of the setup and use of it. I’m grateful for the face-to-face connection. But with video visits I feel the loss of being in a room with someone and having my emotional antennae twitch with a change in emotional valence, from the small barely-discernable welling of tears in someone’s eyes to the escalation of energy emanating from someone in anger or happiness.
And (sigh) the billing. It was so frustrating waiting on insurance providers to allow telehealth visits to be charged, and to be compensated adequately for them, and to discover the disapproval of telehealth sessions across state lines. For me, about three months of charges for weekly telehealth visits with a patient were all rejected because I had not included a statement about the patient agreeing to participate in it. (What, was someone threatening him on the other end to engage in these sessions against his will?) The word “synchronous” is part of the statement I’m supposed to make about this bargain with my client. I don’t think I’ve ever used that word in my life, but now I cut and paste the necessary phrase into every telehealth note. For me, this has felt a bit like a trial by fire. When something works, I feel like I dodged a bullet; when it doesn’t and then someone tells me how it should have been done, I wonder why it wasn’t explained before I made the mistake.
At the same time, telehealth is an incredible gift. I used to think of routine telehealth sessions with clients – especially those in rural parts of Iowa – as a pipe dream. But hey, it happened, and it works! I love that people who formerly might have had to drive an hour to see a therapist, or refused to see the one mental health provider in town because they didn’t want to see neighbors and acquaintances in the waiting room, are now able to see mental health providers while staying in their homes. I think about people not only limited by locale but by disability or an immunocompromised state. I began to see opportunities for the future, if we can advocate for ongoing payment from insurance companies for telehealth visits once in-person sessions become de rigueur again. I also imagine that telehealth would mean mental health providers who need flexibility being able to work from home at least some of the time. In this respect, the pandemic invited something promising and of tremendous benefit to people who have lacked access to mental healthcare before now. And we have responded with remarkable alacrity.
I am seeing more therapy clients now than I was before the pandemic and would imagine that most practices are thriving. It feels like everyone has seasonal affective disorder jacked up on steroids. I’ve noticed that I talk with my patients about the same sort of things we’ve always talked about, but the pandemic seems to sharpen the intensity and clarity of every issue and life stressor. Synchronously, we as providers are also living through this. Clients’ stories might feel more familiar than ever before, because their stories are a lot like our stories. Undoubtedly our empathy is greatly appreciated, but WE don’t get a break.
As the pandemic plodded on into fall, the weight of all of this began wearing on me. I started watching “comfort” TV in the last few months, reruns of shows I’ve seen in reruns many times in the past. Shows like Law & Order and Intervention. I have enough insight to recognize that my choice of blood, gore, violence, and tragic real-life, spinning-out-of-control behavior as comfort TV is weird. I haven’t quite figured this one out, but suspect that it’s kind of a relief to see crazy stuff happening on TV where someone else has to deal with it.
I found myself having a harder and harder time getting out of bed and getting motivated every day as we crept into fall. I have a psychologist with whom I check in regularly (and she has a psychologist, and hopefully her psychologist has a psychologist) and that helped. I’ve been using all the strategies I advise others to use: eating well, staying hydrated, exercising regularly, getting enough sleep, keeping mindful that the negative messages floating through my mind were just words and not truth, and using meditation to regularly reduce the tension that I figured was causing some sort of inflammatory process somewhere. What I haven’t had is the social engagement that is so necessary to keep us healthy. I desperately miss hugs and touch. I found myself growing duller, as if the mask and face shield I wear during the day had become a barrier to accessing my true self at home. I experienced a diminishment of creativity and motivation to do things around the house that I’d found so easy to initiate last year (like my landscaping project). At last, I stopped trying to be invincible and spoke with a psychiatrist about how I was feeling. I’d been loath to consider an antidepressant – because I’m a psychologist, for crying out loud, and I believe heartily in the treatments we provide! – but I acknowledged I could be helped with medication. It made an immediate difference. I’m still doing all the other things (exercising, hydrating, sleeping, meditating, etc.), but now I feel hopeful again, and I’ve been able to tap into the livelier parts of my brain. Importantly, I’ve forgiven myself for not being able to do it all.
Mental health professionals are among the most essential of essential workers for surviving this pandemic, and we’ll be cleaning up the detritus long after most have been able to put away their masks and other weapons against COVID. There will be many healthcare workers traumatized by what they have experienced who will need our help. There will be children who experienced the negative effects of the isolation and lack of needed interventions who will require intense attention for a while. We, as a collective, might be seeking each other’s services to help us carry the burden of helping our clients through what we, too, have suffered.
Though many unknowns still hover before us, I am certain of this: we will rise to the occasion. We chose this profession for a reason, maybe because we have a remarkable capacity for empathy or we love helping others or we are fascinated by each new story we hear. We walk many journeys with our clients, (hopefully) always learning, always growing. We are resilient, as we have already demonstrated in our adjustment to pandemic-induced obstacles, our thriving in the presence of those obstacles. As we move forward, if we rely on each other and allow ourselves to be vulnerable to the moment, we will save our communities and ourselves. I can think of no better synchronous effort than that.






 This story begins in Iowa in the spring of 2021. I had white knuckled my way through the darkest days of the pandemic, doing my best to hold space for and support my clients’ fears, frustrations, anger, and depression while also navigating my own fears, frustrations, anger, and depression. My schedule was booked solid 11 weeks out, which felt suffocating. Many of my clients seemed to be just treading water, which left me feeling ineffective. My mind wandered during sessions. I procrastinated writing my session notes, and they piled up such that there was a mountain of them to do on the weekend. I was easily annoyed by, well, basically everything. I was completely exhausted when I got home at the end of the day. I had no emotional energy for my spouse and family members. I started to dread going to work. I had all the signs of
This story begins in Iowa in the spring of 2021. I had white knuckled my way through the darkest days of the pandemic, doing my best to hold space for and support my clients’ fears, frustrations, anger, and depression while also navigating my own fears, frustrations, anger, and depression. My schedule was booked solid 11 weeks out, which felt suffocating. Many of my clients seemed to be just treading water, which left me feeling ineffective. My mind wandered during sessions. I procrastinated writing my session notes, and they piled up such that there was a mountain of them to do on the weekend. I was easily annoyed by, well, basically everything. I was completely exhausted when I got home at the end of the day. I had no emotional energy for my spouse and family members. I started to dread going to work. I had all the signs of 









 I was fortunate to acquire an academic job directly out of my pre-doctoral internship. However, the downside of this was that opportunities to apply my clinical skills were largely nonexistent, and acquiring the required 1500 hours of postdoctoral licensure hours was a daunting task while embarking on the tenure track. While I had always found academia fulfilling, after two years focusing solely on teaching and research, a level of monotony began to appear, and the lack of opportunities to work with clients began to frustrate me. Not to mention, I dreaded the prospect of having to repeat the same stories from my past clinical work to my students for the next 50 years if something did not change. Accordingly, despite the challenge and risk of adding a new responsibility to an already full workload, I decided to take on a part-time clinical position to complete my licensure hours. Looking back, this was one of the best decisions I have ever made, and the following case exemplifies why I will always have one foot in the clinic.
I was fortunate to acquire an academic job directly out of my pre-doctoral internship. However, the downside of this was that opportunities to apply my clinical skills were largely nonexistent, and acquiring the required 1500 hours of postdoctoral licensure hours was a daunting task while embarking on the tenure track. While I had always found academia fulfilling, after two years focusing solely on teaching and research, a level of monotony began to appear, and the lack of opportunities to work with clients began to frustrate me. Not to mention, I dreaded the prospect of having to repeat the same stories from my past clinical work to my students for the next 50 years if something did not change. Accordingly, despite the challenge and risk of adding a new responsibility to an already full workload, I decided to take on a part-time clinical position to complete my licensure hours. Looking back, this was one of the best decisions I have ever made, and the following case exemplifies why I will always have one foot in the clinic.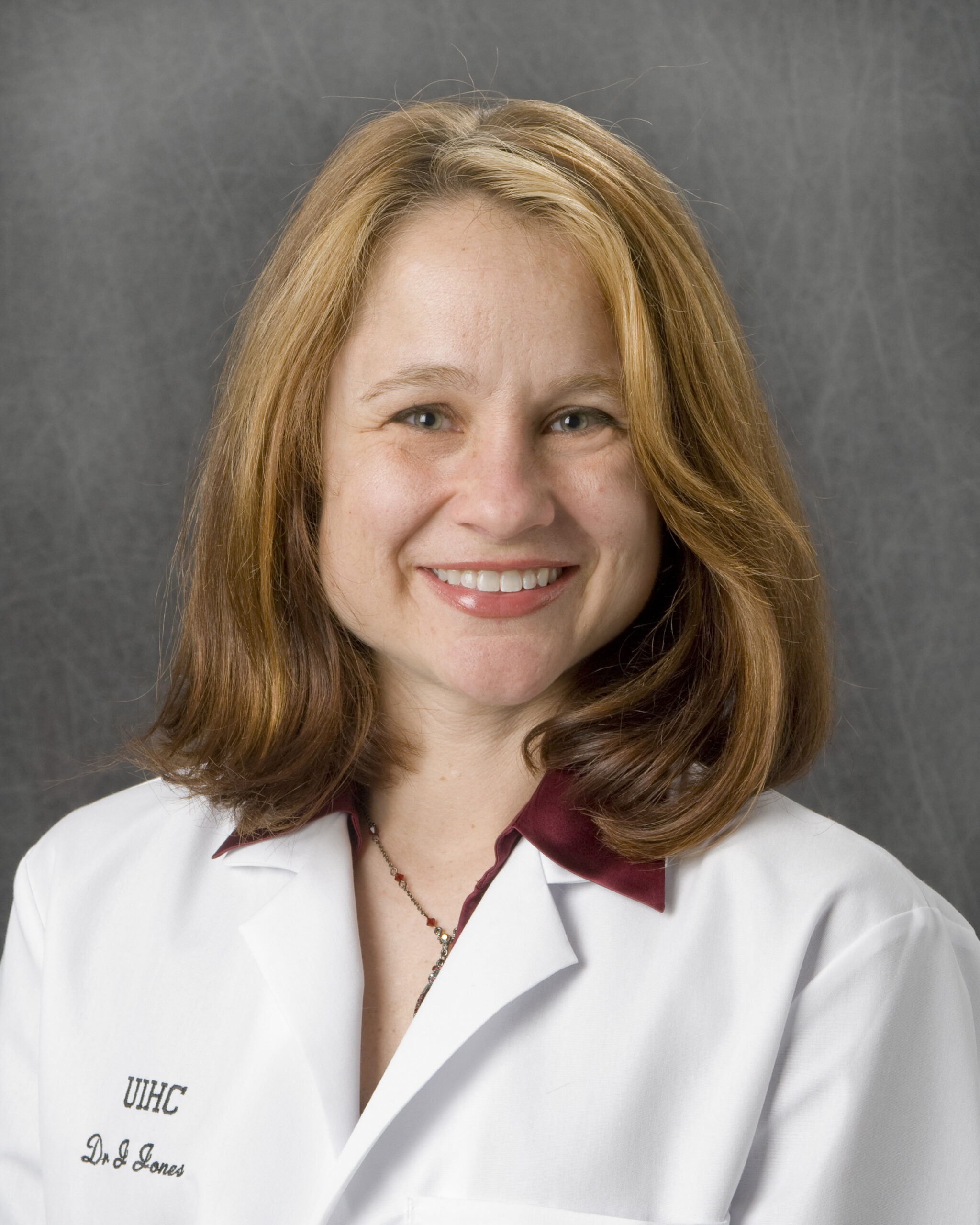
 This is my first blog post ever! I consider this another gift of the pandemic.
This is my first blog post ever! I consider this another gift of the pandemic.